Is Your Back and Leg Pain or Numbness Worse When You Walk or Stand?
H2 SUBHEADING IN THE FORM OF A QUESTION
Do you experience pain, numbness, or heaviness in your back and legs that gets worse the longer you stand or walk, but eases when you sit or lean forward? This pattern is called neurogenic claudication—a hallmark of lumbar spinal stenosis, a common cause of back and leg pain in adults over 50.
What Is Lumbar Spinal Stenosis?
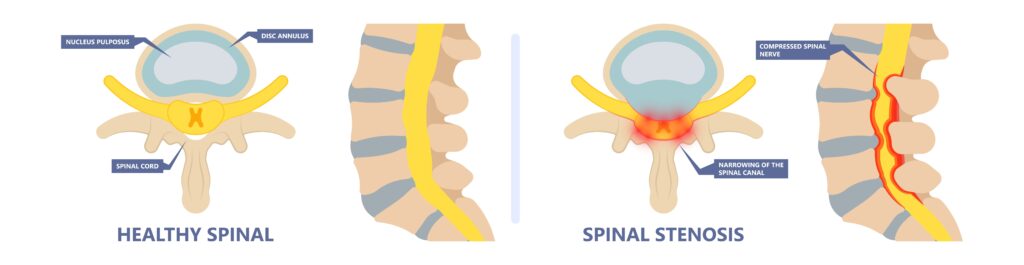
The spinal nerves run through a central canal within the spine, resembling a “horse’s tail” (cauda equina), before exiting the spine through small openings on each side called neural foramina, or nerve holes. Lumbar spinal stenosis occurs when the central canal or these nerve holes (neural foramina) become narrowed, putting pressure on the spinal nerves that travel down into the legs.
This narrowing can develop from disc degeneration, thickened ligaments, bone spurs, or arthritis of the facet joints. As these structures tighten around the nerves, they can compress and irritate them, especially during upright activities such as standing or walking, when the spinal canal naturally becomes smaller.
When you sit or bend forward, the spinal canal and nerve holes slightly open, relieving pressure on the nerves and easing pain or numbness. This is why many people with lumbar stenosis feel better leaning forward or resting on a shopping cart.
Resolve Neck, Back, and Sciatica Pain and Regain Your Function
Symptoms of Lumbar Spinal Stenosis
- Pain, burning, or tingling in the lower back, buttocks, or legs
- Numbness or heaviness in the legs after standing or walking (neurogenic claudication)
- Relief when sitting or leaning forward (for example, over a shopping cart)
- Weakness in the legs or difficulty walking long distances
- Back stiffness or fatigue after activity
How Posture and Weakness Contribute to Stenosis
Spinal stenosis is both a structural and a functional issue.
When the stabilizing muscles and ligaments of the spine are weak, the spine loses its ability to maintain alignment during upright activities. This can cause the canal to narrow even more during standing or walking, worsening symptoms.
Arthritis in the hips and limited hip extension also increase stress on the lower back. When the hips can’t move properly, the spine compensates—putting more pressure on the lumbar segments and aggravating stenosis pain.
Diagnosing Lumbar Spinal Stenosis
Diagnosis begins with a detailed history and physical exam.
Our spine specialists assess posture, flexibility, muscle strength, reflexes, and nerve function, while also checking whether pain increases with standing or walking and improves when sitting—classic signs of stenosis.
Imaging Studies
MRI is the most accurate way to visualize the spinal canal and nerve roots, showing where compression occurs. X-rays or CT scans may be used to evaluate bone spurs, alignment, or joint changes. However, imaging is always interpreted alongside your symptoms and exam findings.
Non-Surgical Treatment of Spinal Stenosis
Why Conventional Treatments Often Fall Short
Traditional care for spinal stenosis usually involves steroid epidural injections to calm inflammation. These can offer short-term relief, but they don’t address some of the contributing issues such as ligament laxity, disc degeneration, or instability. Frequent steroid use may also cause elevated blood sugar, muscle loss, and bone thinning (osteoporosis), while doing little to improve long-term spinal health.
Regenerative Medicine: A Functional, Healing Approach
At Integrative Rehab Medicine in Estero, Florida, we focus on restoring stability, mobility, and tissue health—treating the root cause instead of masking symptoms.
All procedures are performed under fluoroscopy or ultrasound for precision and safety.
PRP Epidural Injections (Lysate or Releasate)
PRP lysate delivers healing growth factors from your own platelets directly around irritated nerves. This helps reduce inflammation, support nerve repair, and make nerves more resilient to compression.
Prolotherapy and PRP for Ligaments and Muscles
Weak ligaments and muscles can make stenosis worse. Prolotherapy and PRP strengthen these tissues, improve spinal support, and reduce nerve stress during movement.
Discseel® Procedure (for Select Cases)
When leaking or degenerated discs contribute to inflammation and nerve irritation, the Discseel® procedure can seal tears and restore disc integrity. It’s best suited for disc-related cases without severe canal narrowing.
Collaborative Treatment for Spinal Stenosis
Regenerative treatments work best when combined with spinal and pelvic physical therapy focused on core stability, hip mobility, and posture correction. Strengthening the hips and spine helps relieve pressure on the nerves and restores endurance during upright activities.
We also emphasize lifestyle habits that support healing:
- Maintaining a healthy weight to reduce spinal load
- Quitting smoking to enhance circulation and tissue repair
- Following an anti-inflammatory diet rich in nutrient-dense foods
Sometimes, even with the best regenerative and rehabilitation treatments, symptoms may not fully resolve. In such cases, a surgical decompression may be necessary to relieve pressure on the spinal nerves and restore proper function. Once the nerves are freed from compression, regenerative treatments and targeted rehabilitation may be also utilized to strengthen the spine and support long-term recovery.
That’s why collaboration is essential in treating spinal stenosis. At Integrative Rehab Medicine, we work closely with expert spine surgeons in Southwest Florida who specialize in spinal stenosis decompression procedures, ensuring our patients receive comprehensive, coordinated care tailored to their individual needs.
Resolve Neck, Back, and Sciatica Pain and Regain Your Function
Frequently Asked Questions
Spinal lumbar discs are strong but their weakness is when they are loaded and twisted, with a forward flexion and rotation movement, such as lifting a heavy bag and placing it into a car. Repetitive tasks that require a flexed forward position and also wear down the outer layer of the disc (annulus), cause cracks that will eventually lead to a disc herniation. Trauma such as car accidents and falls can also place enough force onto the disc to cause a herniation,
Just like all the tissues in our body, spinal disc herniations have the ability to heal on their own. The body sees the herniated disc material as an intruder and sends out immune cells such as the macrophages to “eat up” the disc material. This healing can be a slow process and can happen on its own, but it does not always occur and often the body needs a reminder to heal the disc herniation. There are many other alternatives to surgery for a herniated disc, such as ozone and PRP epidural injections that can stimulate the body to heal the disc herniation.
A large enough herniated disc can compress nerves in the spine and cause nerve damage, especially if not treated quickly. If there is severe pain and significant weakness, the disc herniation needs to be addressed ASAP in order to save the nerves from long lasting damage.
Yes, a herniated disc can compress nerves within the spine, cutting of blood supply to the nerve and causing direct damage to the nerve tissue itself. This can cause long term nerve damage if not addressed properly.
A bulging disc is when the outer layer of the disc (the annulus) becomes weak and bulges out in all direction causing the disc to flatten and expand. A herniated disc is when some of the inner core material (the nucleus) leaks out through the annulus in one direction, causing nerve compression and inflammation.
Most important way to prevent a herniated disc from coming back it to create a strong and stable spine. This can be done with specific core exercises, rebuilding of the muscles and strengthening of the ligaments (such as can be achieved with prolotherapy and PRP injections). The other important thing is to follow “spinal hygiene” – avoiding activities that can place excessive load on the disc – such as flexion and rotation positions.
If you have back pain and pain in the leg (aka sciatica) that is worse with sitting, bending and walking, along with some numbness and weakness in the leg, you may have a herniated disc. Sometimes there may be no back pain and only leg symptoms are present.
Many times disc herniations can be treated without surgery using therapy, injections of ozone or PRP and time. If you have severe weakness and pain that does not improve with conservative treatments, then surgery may be indicated.
A spinal MRI is the best way to visualize a disc herniation. X-ray will not a disc herniation. A CT scan can also be used but it is not as good as an MRI.
Resolve Neck, Back, and Sciatica Pain and Regain Your Function
Why Choose Integrative Rehab Medicine
At Integrative Rehab Medicine in Estero, Florida, we specialize in non-surgical regenerative spine care designed to restore function and prevent recurrence.
Patients choose us because we offer:
- Board-certified regenerative spine specialists with national recognition
- An in-house biologics lab for the highest-quality PRP preparation
- Image-guided precision for every injection
- Integrated rehabilitation and nutrition programs for whole-body recovery
If you’re ready to move beyond short-term pain relief and address the true cause of your spinal stenosis, our team is here to help you regain strength, mobility, and confidence in your movement.
Contact Integrative Rehab Medicine today to schedule your consultation.
With more positive improvement coming long term my advice why wait call or visit them. Integrative Rehab Medicine is the very best non-surgical treatment of the spinal discs.
I excited about my future living without pain. Make this appointment your health will Thank you later.
Chris Drikakis
A fellow golfer and Vietnam veteran
We’re thrilled to hear that just one month after your non-surgical spinal disc procedure, your consistent pain has resolved and that you’re continuing to make progress. At Integrative Rehab Medicine, our mission is to help patients avoid unnecessary spine surgery by offering advanced, evidence-based treatments for chronic back and neck pain, including non-surgical disc repair options such as Discseel® and PRP.
Your story highlights exactly why we focus on treating the underlying cause of disc-related pain—not just masking symptoms—and why so many active patients, including golfers and veterans, seek out non-operative spine care with us. We’re excited about your continued improvement and long-term recovery.
https://irehabmed.com/va
Thank you again for your kind words.
We’re thrilled to hear that your ozone intradiscal treatment combined with lysated platelet (PRP) epidural injections helped you avoid a major back surgery and a prolonged recovery. At Integrative Rehab Medicine, we love helping patients with herniated and bulging discs find effective, non-surgical alternatives to spine surgery.
Your outcome highlights the power of biologic and regenerative spine treatments—using ozone to reduce disc inflammation and herniation, along with platelet-based therapies to support healing around irritated spinal nerves. We’re also glad to hear your experience with Kristine, our physical therapist, has complemented your recovery.
Thank you again for your words and confidence in our team.
While Discseel® can be an excellent option for certain patients, we’re glad you found success with platelet-rich plasma (PRP) and prolotherapy—two powerful non-surgical treatments designed to reduce inflammation, support tissue healing, and improve spinal stability. As you experienced, biologic spine treatments often require patience, with healing occurring over weeks to months, but the long-term improvement can be life-changing.
We’re especially happy to hear that you’re now pain-free and that movements which once caused months of setback now result in only brief, mild discomfort. That kind of functional recovery is exactly what we aim for at Integrative Rehab Medicine.
We truly appreciate the recommendation and are honored to be part of your long-term spine health.
Thank you Integrative Rehab Medicine for changing my life
It’s wonderful to see your body responding and healing after so many years. Thank you for trusting us with your care!
We appreciate you sharing your experience and are honored to be part of your recovery journey!

