Study:
A prospective randomized clinical trial (Hassanien et al., Pain Medicine, 2020) evaluated ultrasound-guided perineural PRP for painful diabetic peripheral neuropathy (DPN).
Sixty adults with type 2 diabetes and at least 6 months of symptomatic DPN were randomized to PRP plus standard medical therapy vs medical therapy alone. Outcomes included pain VAS, numbness VAS, modified Toronto Clinical Neuropathy Score (mTCNS), and nerve conduction studies (NCV) at 1, 3, and 6 months.
Results:
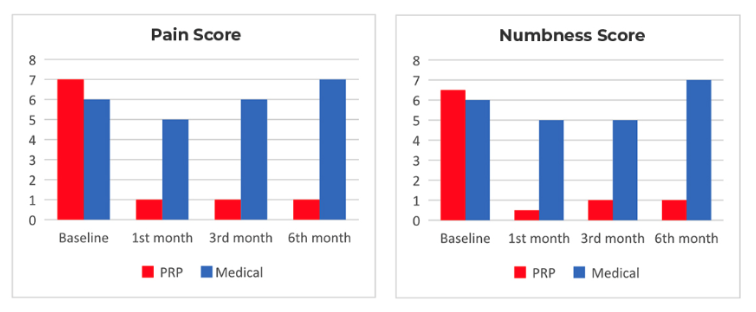
- The PRP group showed significant reductions in pain and numbness at 1, 3, and 6 months compared with the control group.
- mTCNS improved in the PRP group at all follow-up points, indicating better sensory function.
- Nerve conduction velocities increased in both upper and lower limb nerves at 6 months in the PRP group.
- Improvement began within the first month and continued through the full 6-month trial period.
- Safety profile was excellent, with only mild, transient soreness or paresthesia in a few patients and no serious adverse events.
Key Takeaway:
A single ultrasound-guided perineural PRP session added to standard care provided sustained improvements in painful diabetic neuropathy, reducing pain and numbness while also improving objective nerve conduction measures. This targeted, autologous treatment offers a promising option for patients who continue to experience symptoms despite medication.
At Integrative Rehab Medicine, we collaborate with local physical therapy practices to pair regenerative healing with targeted rehabilitation, optimizing recovery, biomechanics, and long-term outcomes.
Reference:
Hassanien M, Elawamy A, Kamel EZ, et al. Pain Medicine (2020); 21(4):757–765.
“Perineural Platelet-Rich Plasma for Diabetic Neuropathic Pain, Could It Make a Difference?”
https://pubmed.ncbi.nlm.nih.gov/31298289/
