Study:
A landmark study published in Pain Physician (Pauza et al., 2024) evaluated 827 patients with chronic low back pain lasting over six months (average duration 11 years). All patients had failed at least four prior invasive treatments, such as epidural or facet steroid injections, PRP or stem cell therapy, radiofrequency ablation, and even spinal surgery, including discectomy or fusion.
Each patient underwent an annulogram to identify leaking discs before receiving targeted intra-annular injections of fibrin sealant (Discseel Procedure). The fibrin biologic acts as a bio-adhesive that seals annular tears, prevents disc fluid leakage, and promotes new tissue growth within the disc.
Results:
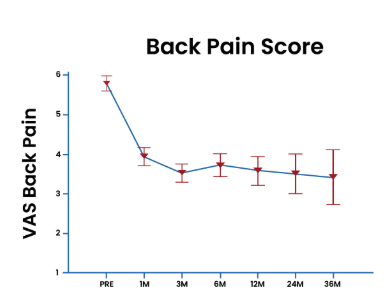
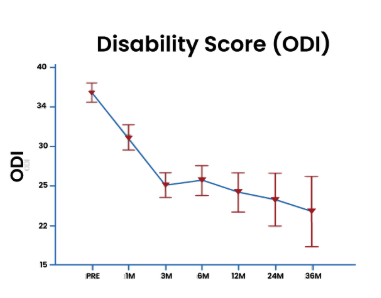
- Significant improvements in back and leg pain, disability (ODI), and quality of life were seen within 3 months and continued to improve at 1, 2, and 3 years.
- About 70% of patients reported satisfaction with their Discseel® treatment at long-term follow-up.
- Even patients who had prior spinal surgery (fusion or discectomy) showed meaningful pain reduction and functional gains.
- No serious complications or adverse events were reported during the study.
- Improvements were consistent across both surgical and non-surgical subgroups, confirming safety and durable efficacy.
Key Takeaway:
Fibrin sealant injections via the Discseel® Procedure safely and effectively treat chronic discogenic back pain and radiculopathy—even in patients who have failed multiple prior treatments. The study demonstrates durable improvements in pain, function, and quality of life up to three years post-procedure, highlighting fibrin’s unique regenerative and sealing properties.
At Integrative Rehab Medicine, the Discseel® Procedure is combined with PRP treatment of the facet joints, ligaments, muscles, and fascia to treat the whole spinal unit. We combine this biologic repair with post-procedure rehabilitation and close collaboration with local physical therapy providers to help patients restore spinal stability, movement, and long-term function.
Reference:
Pauza, K. et al., Pain Physician (2024); 27:537–553.
https://www.painphysicianjournal.com/current/pdf article=NzkxOQ%3D%3D&journal=166
